Background: Patients with sickle cell disease (SCD) have reduced life expectancy and high morbidity, despite treatments such as hydroxyurea, transfusion, vaccination, and antibiotic prophylaxis. Both allogeneic hematopoietic stem cell transplant (HSCT) and more recently, gene therapy (GT) via ex vivo manipulation of autologous hematopoietic stem cells (HSC), have emerged as curative strategies for SCD. However, both therapies carry significant risks. HSCT and GT have both demonstrated efficacy against SCD in clinical trials, but have not been compared. Here, we present the updated results of a systematic review comparing HSCT and GT in SCD.
Methods: We searched the MEDLINE and EMBASE databases for studies reporting HSCT and GT outcomes in SCD. Phase I-III trials, retrospective reviews, and case reports with >1 SCD patient undergoing HSCT or GT were included. All HSC donor types and conditioning regimens were included. References of included studies were screened for additional relevant studies. All titles/abstracts were screened for full text retrieval. Non-English and preclinical studies were excluded. Primary outcomes were overall survival (OS), event-free survival (EFS), graft failure, transplant-related mortality (TRM), graft-versus-host disease (GVHD), and secondary malignancies. Secondary outcomes were end-organ function, acute chest syndrome/vaso-occlusive episodes (ACS/VOE), and health-related quality of life (HRQOL). We used descriptive statistics to analyze data on study characteristics, quality, and effects. Risk of bias was assessed using the Newcastle-Ottawa Scale. Outcome heterogeneity was assessed using sensitivity and subgroup analyses. Publication bias was assessed with funnel plots, where applicable.
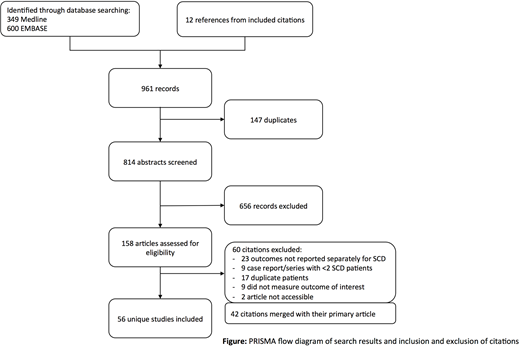
Results: We identified 949 titles through database searching and 12 titles from references of included studies (Figure). After removal of duplicate citations (n=147), exclusion of ineligible records (n=716), and merging 42 studies with their primary article, 56 studies were included for data extraction. Of these 56 studies, 53 reported outcomes post-HSCT (n=1149) and 3 reported outcomes post-GT (n=28). Length of follow-up was 3718.6 patient-years and 43.4 patient-years in the HSCT and GT groups, respectively. Median age was 11.5 across HSCT studies; 26/28 GT patients were >18 years. HSCT donor source was matched related donor (n=812), matched unrelated donor (n=73), haploidentical (n=127), or mismatched unrelated donor (n=11) among 1023 HSCT patients.
Two-year OS and EFS for HSCT was 91% and 87%, respectively. OS and EFS were not reported for GT studies. TRM was 74/1042 (7.1%) over a median of 3 years of observation for HSCT, and 0/28 (0%) over a median of 1.6 years of observation for GT. Secondary malignancies were reported in 4 SCD patients from the HSCT group and 1 SCD patient from the GT group.
While the vast majority of HSCT studies reported the absence of ACS/VOE in engrafted patients, the lack of published data on pre- and post-transplant ACS/VOE frequency precluded further analysis. Median annual ACS/VOE episodes decreased from 5.3 to 0 post-transplant in 1 GT study, while a second GT study reported 2 episodes of ACS and 1 VOE post-GT. Fourteen studies (n=375), all from the HSCT group, reported 6 strokes/TIAs out of 2030.5 patient-years of post-transplant follow-up, with 1/6 strokes occurring in engrafted patients. None of the GT studies explicitly commented on stroke as an outcome. Only 1 study quantified changes in tricuspid regurgitant jet velocity post-transplant, and 1 study reported on renal function pre- and post-transplant, both from the HSCT group. There was no change in pulmonary function testing values post-transplant, as reported by 2 HSCT studies. Post-transplant HRQOL was reported for 8 HSCT studies and 0 GT studies, but due to heterogeneity of reporting, meta-analysis could not be performed.
Conclusions: While long-term HSCT and early GT data demonstrate regimen efficacy, reporting of other important post-transplant outcomes such as end-organ function, persistence of SCD-related complications, and patient-important outcomes is lacking for both strategies. Small sample sizes and differential reporting of outcomes preclude comparison between subgroups of HSC sources and conditioning regimens, a limitation of our study. We advocate for standardized reporting to better compare outcomes within and between treatment groups.
Kuo:Celgene: Consultancy; Pfizer: Consultancy, Research Funding; Alexion: Consultancy, Honoraria; Novartis: Consultancy, Honoraria; Bioverativ: Membership on an entity's Board of Directors or advisory committees; Agios: Consultancy, Membership on an entity's Board of Directors or advisory committees; Bluebird Bio: Consultancy; Apellis: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.